Who Needs It?
Who benefits from MTM?
All who uses drugs can benefit from MTM. This helps evaluate the drugs being taken and reviews interactions and side effects
that may be happening around intake:
- - Prescription medications
- - Non-prescription medications
- - Herbals
- - Dietary supplements could probably benefit from medication therapy management services
Maximum benefit is to persons who are
- - Take multiple medications
- - Persons with several health conditions
- - Address questions or problems of consumers with their medications
- - Persons on medications that require close monitoring
- - Those who have been hospitalized
- - Medications from multiple physicians or more than one pharmacy.
What Problem MTM Solves?
HIGH HEALTHCARE COSTS: World Health Organization, findings show that medical aid for chronic diseases in
developed countries averages 50%,
and therefore the consequences of poor drug medical aid cause health outcomes and increased health care costs.”
The two most common drug medical care problems experienced by patients receiving comprehensive medication management are that MTM solves:
- - The patient requires additional drug medical aid for prevention, synergistic or palliative care.
- OR
- - The current drug dosages need to be titrated to achieve therapeutic levels that reach the intended goals of therapy.
Patients With Chronic Disease Are At High Risk
Persons with multiple chronic illnesses:
- - On an average see 13 different physicians
- - Fill 50 different prescriptions per year
- - Account for 76% of all hospital admissions
- - Are 100 times more likely to have a preventable hospitalization than someone with no chronic conditions.
The Institute of Medicine has noted that while only 10% of total healthcare costs are spent on medications, whereas they have
ability to control disease and impact overall cost, morbidity, and productivity–when appropriately utilized–is enormous.
“Pharmaceuticals are the most common medical intervention, and their potential for both help and harm is enormous. Ensuring that the American
people get the most benefit from advances in pharmacology is a critical component of improving the
national health care system.” Institute of Medicine.
Which patients benefit most from comprehensive MTM?
The Connected Collaborative Care Technology is especially helpful if you, your partner, parent or child have a chronic illness or are
recovering from surgery and take multiple medicines.
Significant evidence is there to establish (+) ve impact on patient health and achieve improved health, lowers morbidity, longer life & better
outcomes through comprehensive medication therapy management.
Patients segments that benefit the most:
- - Patients reaching or are not maintaining the intended goal of therapy
- - Patients who are experiencing adverse effects from their medications
- - Patients who have difficulty in understanding and following their medication regimen
- - Patients in need of preventive therapy, and
- - Patients at risk of hospital re-admission
Chronic Disease Patient Drives Maximum Benefit:
Chronic Diseases which are costly and are associated with multiple medications to control them are great candidates to drive
maximum benefits. They are:
- - Diabetes
- - Cardiovascular disease, (Hypertension, CHF etc.)
- - COPD
- - Asthma (in children)
- - Obesity & Hyperlipidemias
- - Cancer chemotherapy
- - Depression
- - Pain management and
- - Hypothyroidism
MTM Solution Offering
MTM is an integral part of the Managed Care services offering. The personal care team has Pharmacist/ Pharmacologists along with
Care coordinators, Doctors and Specialists. They undertake a review of medications under the guidance of a Pharmacologist periodically.
Patient Enablement: The integrated Drug Database helps provide patients with crisp information from A to Z of the medicine.
The Solution Helps Address The Problems In MTM
The MTM solution helps meet the 7 R’s of medication
- - Take the right medicine
- - For the right ailment
- - By the right person
- - In the right amount
- - At the right time
- - In the right way (swallow, chew, apply to the skin, etc.)
- - With the right diet
Active Wellness Smart MTM Solution is answers to your health questions like
- - Why doctor has given this medicine
- - How much should be taken and when should it be taken
- - What food items are not to be consumed with the medicine
- - What other medicines cannot be taken with the prescribed medicine
- - What are the possible side effects
- - How to manage the side effects
- - In what health states should certain medications be avoided?
Why MTM Is Critical?
DRUGS: We all know that there are now 10,000 prescription drugs and 300,000 over-the-counter medicines in the market.
It is not possible for a human being to manage such a huge repository and thus it requires reliance on technology and analytics
to manage the drug therapy of a person. A Collaborative Connected Platform of Active Wellness is the answer.
The Lurking Danger:
Eight out of Ten adults self-medicate using over-the-counter (OTC) medicines
50% of people have difficulty in
understanding the prescription.
BY LAW when a physician prescribes drugs for a patient, the physician has to make sure that the patient is well informed
of the drugs risks, benefits and correct way of consuming drugs.
- Statistics show that this occurs in less than 20% of the patient population.
- Either doctors are short of time or patients are not in a position to understand what physician is
hurriedly explaining to them.
- Or to make the matter still worse they don’t know what questions to be asked to ensure correct and effective
consumption of medicine.
- Unfortunately, many people don’t consult their doctor, pharmacist or nurse, or take the time to learn about
how to use OTC and prescription medicines safely.
Impact Of Lack Of Knowledge: – 30-50% of prescriptions are not taken as they should be. We are hurt by
Preventable medication errors.
MTM Solution Addresses the need of these 30% – 50% of the cases
- Solves Drug Compliance Issues
- We forget to take medicine.
- Forget to carry them with us while going out/to work.
- Skip for Non-Availability of prescribed medicine in the market
- Decide to Discontinue the medicine before course completion
- Reduce the dose to avoid perceived side-effects or reduce cost
- Helps Avoid Medication Interactions
- Drug – Drug Interactions: Alerts you when try and combine medicines which should not be taken together
- Drug – Food Interactions: Alerts you when you consume medicine with certain food items which should not be taken
with a medication.
- Warns when drugs are Contraindicated based upon health profile
- Alerts consumers when Medication are to be avoided in certain health state or disease.
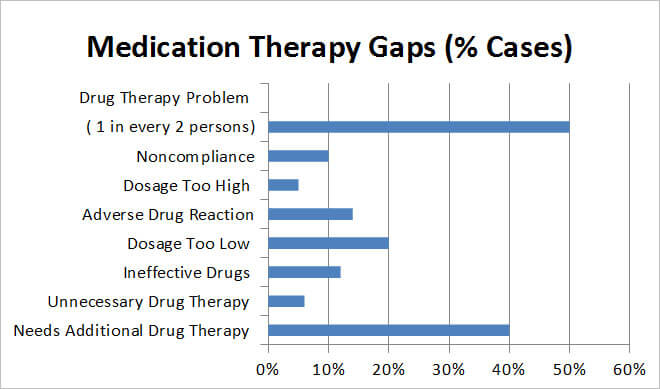
MTM Solution Prevents Common Gaps In Drug Rx
Medication gaps accounts of over 13 % of the medication-related adverse events is listed below. The Smart MTM addresses these and
saves not only money but also improves your health and better control of the disease. MTM closes the following medication gaps.
Beneficial Outcome Of MTM Therapy
When the above gaps in medication are addressed the following objectives are met:
- - Better Control of Disease leading to reduced costly Medical emergencies and Hospitalizations.
- - Reduces Medications that are very common.
| MTM MANAGEMENT PRINCIPLE |
DESCRIPTION OF PRINCIPLE |
CONTRIBUTION OF MEDICATION |
| Personal Relationship with own Physician or Other Licensed Practitioner |
Each person has an ongoing relationship with a personal Care Team of physicians or other licensed healthcare practitioners
who looks after his care. |
The therapeutic relationship is established as through a team approach and continuous monitoring of the patient’s
medication experience through tools is reviewed. This leads to improved care and better health outcomes. |
Team Approach
A Comprehensive Care Team |
The personal physician leads a team at the practice level who collectively take responsibility for the
ongoing care of patients, including disease and/or case management. |
The rational decision-making process for drug therapy is utilized and the assessment, care plan and follow-up of drug
therapy is integrated with the team’s efforts |
Comprehensive/
Whole Person Approach |
The personal physician or other licensed healthcare practitioner is responsible for coordinating and / or providing
for all the patient’s health care needs or taking responsibility for appropriately arranging the same. |
The patient is engaged and empowered in their use and understanding of the medications prescribed in their therapy.
All of a patient’s medications (regardless of source) are coordinated, evaluated, appropriate, effective,
safe and convenient- linked to clinical outcomes and improved health. |
| Coordination and Integration of Care |
Care is integrated and coordinated across all domains of the health care system. |
The intended therapeutic goals, established by different treating Physicians are coordinated and tracked.
These are made measurable and individualized for every patient's needs. The outcome is coordinated and integrated
care for the patient with other team members. |
| Hallmark: Quality and safety |
Quality and Safety are hallmarks of the Personal Coordinated care by the Primary Care Team. |
The Healthcare team review Medication. Drug therapy problems are identified, escalated to the Comprehensive Care Team,
resolved and adverse events prevented in a systematic and comprehensive manner. A coordinated and Collaborative effort
ensures that the patient gets appropriate, effective, safe and convenient drug therapy. |
| Expanded Access to Care |
Enhanced access to care. Escalation Matrix in real time. |
Physicians get to see the Medication Alerts. They can look at the problems and resolve them. This allows the Care team
to be more efficient, and more effective through the optimal management of a patient’s medications. |
| Added Value Recognized |
Enhanced Therapeutic Value |
Improved clinical outcomes, return-on-investment is positive, acceptance by patients is high, and physicians
support the practice. |
Sign Up Form MTM Service
The Connected Care Collaborative Ecosystem has built in MTM management Services and helps to reduce / eliminate the medication gaps.
This service is available under Paid Service.
Self Managed Package:
Here you can manage your medication through the platform by entering your drugs and receive medication alerts.
There is no specific comprehensive review. The platform allows you to request medication review as additional services.
Sign in to Know more...
Managed Care Packages:
Here you get to have a “Personal Care Team” that help manage your medications. The Care Team works with you for bettering your
health 24x7x365. The team through use of built in intelligence and medical expertise manages the medications and identifies
gaps in care. It helps you stay healthy and keep your medical conditions under control.
Sign in to Know more...
Home Care Management:
We offer MTM services to patients that have multiple Chronic Conditions and have been discharged from hospital. We offer them care
service at home. Please leave a message and we will contact you.